- What is E-Prescribing Software?
- How E-Prescribing Software Works Step by Step
- Key Features of Modern E-Prescribing Software
- Benefits of E-Prescribing Software for Healthcare Providers
- Who Uses E-Prescribing Software and Why
- When Custom E-Prescribing Makes Sense
- Regulations and Compliance for E-Prescribing Software
- Challenges of E-Prescribing Software
- Future of E-Prescribing Software
- How to Choose the Right E-Prescribing Software
- Conclusion
- Frequently Asked Questions (FAQs)
Table of Contents
What Is E-Prescribing Software and How It Works

Paper prescriptions are slowly giving way to smarter digital systems, and for good reason.
Today, physicians and healthcare providers need faster, safer ways to manage prescriptions without paperwork, callbacks, or avoidable errors.
That’s where e-prescribing software comes in.
Simply put, electronic prescribing software allows doctors to send prescriptions digitally to pharmacies using secure eRx systems.
It reduces prescription errors, improves medication management, and supports patient safety through built-in checks and compliance standards.
What once required complex Electronic Health Records is now available through lightweight, cloud-based healthcare software.
This guide explains what e-prescribing is, how electronic prescribing systems work, and how clinics and hospitals can adopt e-prescribing software effectively within modern healthcare workflows.
What is E-Prescribing Software?
E-prescribing software is a digital system that enables physicians to send prescriptions electronically to pharmacies, eliminating paper, fax, and phone calls.
It improves speed, reduces prescription errors, and strengthens patient safety through automated drug interaction checks.
Modern electronic prescribing systems operate on secure eRx networks and follow HIPAA and DEA compliance standards.
Many platforms also support Electronic Prescriptions for Controlled Substances (EPCS) through additional verification.
In today’s digital healthcare workflows, e-prescribing software has become a faster, safer alternative to traditional prescription methods.
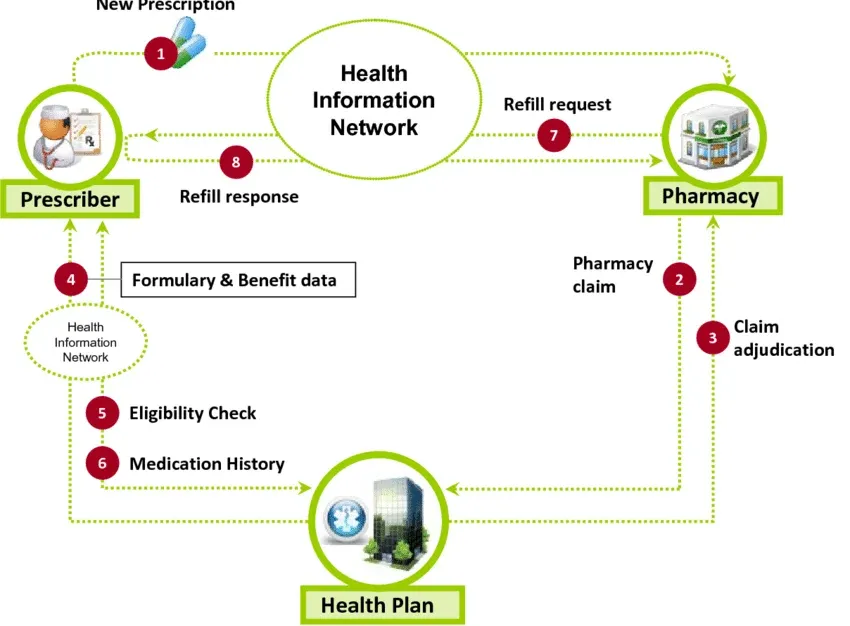
How E-Prescribing Software Works Step by Step
E-prescribing software is designed to fit smoothly into everyday clinical workflows. Below is a clear, real-world breakdown of how e-prescribing works from start to finish.
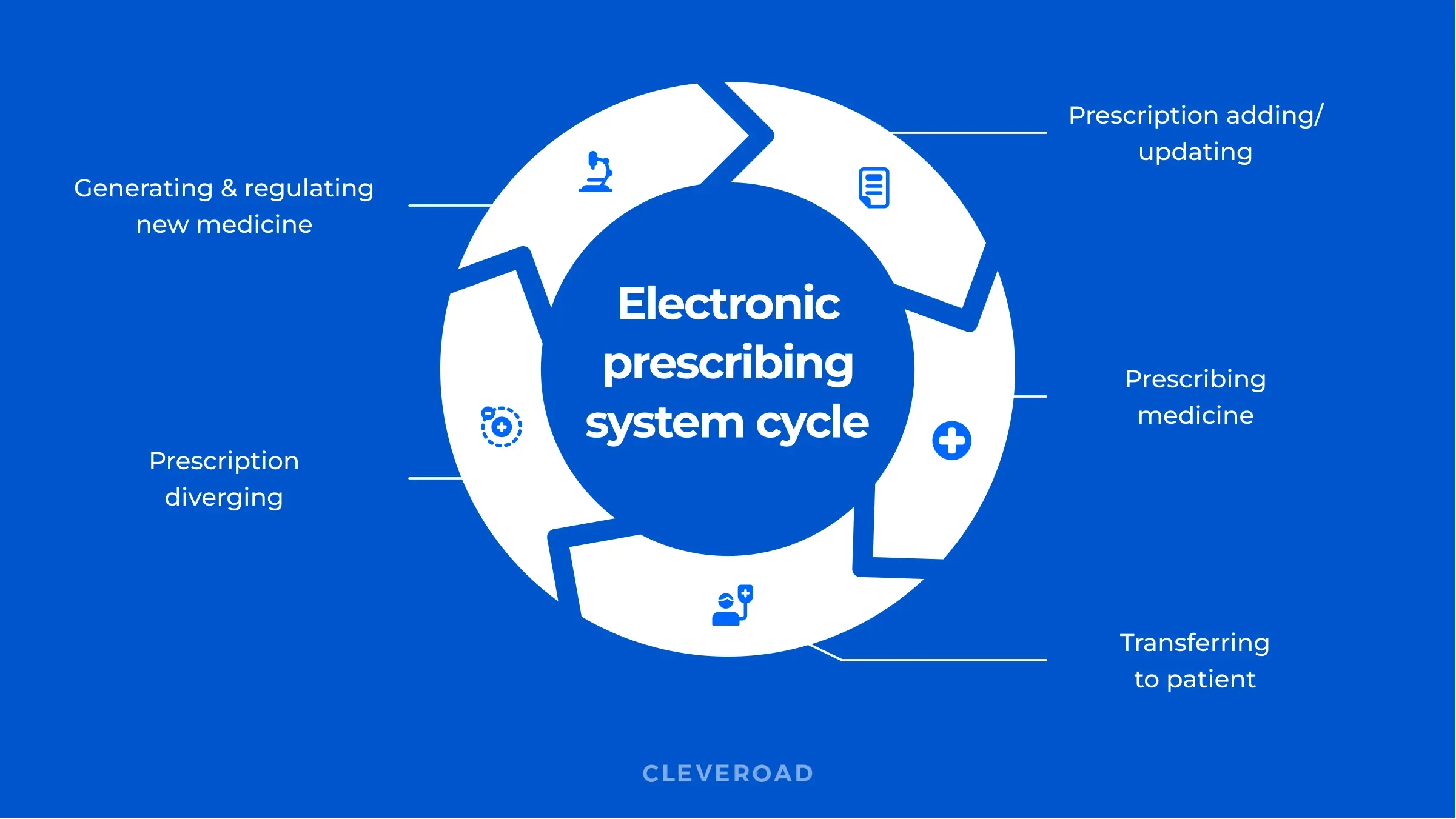
Prescription Entry
Physicians log in to the electronic prescribing system, search for the medication, and select the dosage, frequency, and number of refills using updated drug databases.
Automated Safety Checks
The e-prescribing software runs drug interaction checks, allergy alerts, and duplicate medication reviews to reduce prescription errors and protect patient safety.
Compliance Verification
Prescriptions are validated against HIPAA and DEA regulations, with additional authentication for Electronic Prescriptions for Controlled Substances (EPCS) when required.
Secure Transmission
The approved prescription is sent electronically through secure eRx systems, often via the Surescripts network, directly to the patient’s chosen pharmacy.
Pharmacy Fulfillment
Pharmacists receive a clear digital order, prepare the medication, and notify the patient for pickup or delivery.
Patient Access
Patients collect their medication without paperwork, delays, or follow-up calls.
This step-by-step process shows why electronic prescribing software has become essential for clinics, hospitals, and modern digital healthcare workflows.
Key Features of Modern E-Prescribing Software
Modern e-prescribing software goes far beyond replacing paper prescriptions.
It functions as a connected system that enables safer decisions, faster workflows, and improved coordination among physicians, clinics, and pharmacies.
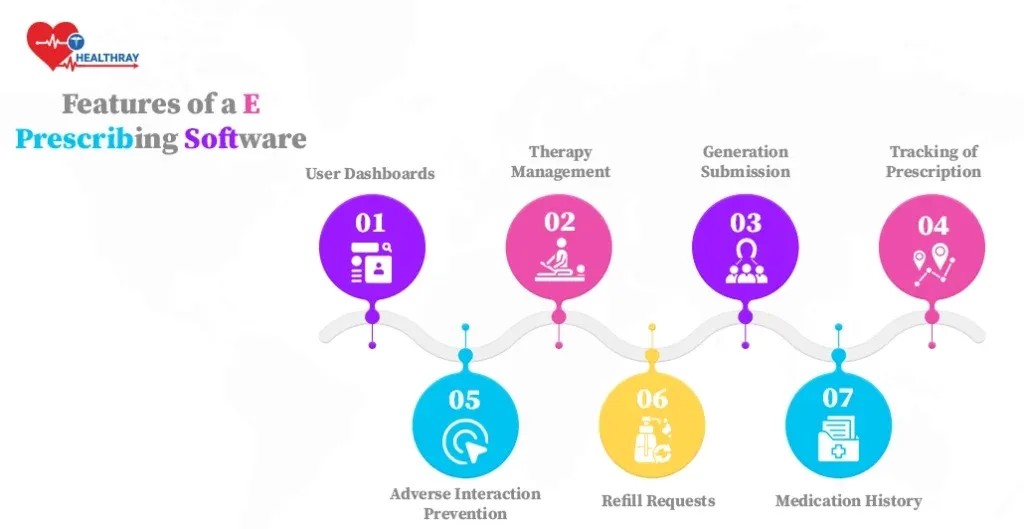
Here are the core features that define reliable electronic prescribing software today:
Drug Database Access
Physicians can quickly search medications, strengths, and forms using updated drug libraries, reducing the risk of outdated or incorrect prescriptions.
Drug Interaction and Allergy Checks
Built-in checks automatically flag potential interactions, allergies, or duplicate medications, helping prevent prescription errors and improve patient safety.
Digital Signatures
Prescriptions are signed electronically and securely, ensuring compliance with legal and regulatory requirements while speeding up delivery to pharmacies.
Refill and Renewal Management
Patients can request refills digitally, and providers can review and approve them quickly, supporting consistent medication management for long-term care.
EHR Integration
E-prescribing software integrates with Electronic Health Records (EHRs) to ensure medication data, diagnoses, and visit notes remain synchronized across digital healthcare workflows.
Together, these features make electronic prescribing a dependable, scalable solution for modern healthcare providers.
Benefits of E-Prescribing Software for Healthcare Providers
The real value of e-prescribing software shows up in everyday practice. Beyond convenience, it delivers measurable improvements in how physicians, clinics, and pharmacies work together.
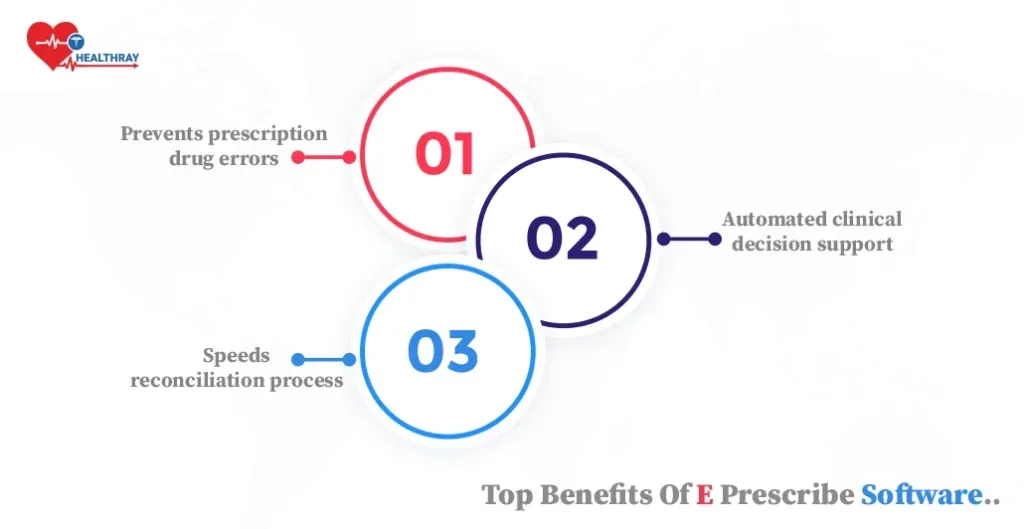
Saves Time
Electronic prescribing software reduces the need for writing, faxing, and follow-up calls.
Prescriptions are created and sent in seconds, helping providers see more patients without added administrative load.
Improves Accuracy
Standardized digital prescriptions eliminate handwriting issues and reduce dosage or formulation mistakes, lowering the risk of prescription errors.
Enhances Patient Safety
Built-in drug interaction checks, allergy alerts, and validation steps help catch risks early and support safer medication decisions.
Improves Patient Experience
Patients spend less time waiting at pharmacies and can manage refills digitally, making ongoing care smoother and more convenient.
Boosts Operational Efficiency
E-prescribing software streamlines medication management, reduces staff workload, and supports consistent workflows across modern electronic prescribing systems.
These benefits make electronic prescribing for physicians and healthcare providers an essential part of efficient, safe, and scalable care delivery.
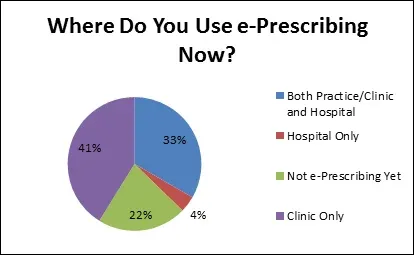
Who Uses E-Prescribing Software and Why
E-prescribing software has become widely adopted because it helps healthcare providers reduce errors, speed workflows, and improve patient safety.
In fact, adoption of electronic prescribing systems is growing rapidly, with digital prescriptions replacing paper and fax methods across clinics and hospitals.
Doctors and Specialists
Physicians use e-prescribing software to send prescriptions directly to pharmacies within seconds, reducing administrative work and callbacks.
Studies show digital prescribing significantly reduces errors caused by illegible handwriting and improves workflow efficiency.
Pharmacies
Pharmacists benefit from clear electronic prescriptions that eliminate interpretation errors and help speed up processing.
Data from national networks shows that high-volume prescription exchanges have shifted toward digital formats, reducing manual handling and improving turnaround.
Clinics and Hospitals
Clinics and hospitals adopt electronic prescribing to manage high prescription volumes across departments, reducing errors and improving coordination.
Reports indicate that digital systems reduce medication misinterpretation and help integrate data across care teams, enhancing overall clinical workflow.
These real-world patterns show that e-prescribing software is no longer a niche technology; it is a core tool for safe, efficient, and modern healthcare delivery.
When Custom E-Prescribing Makes Sense
Standard e-prescribing software works for basic needs, but many healthcare providers require systems that reflect how their teams actually operate.
Custom electronic prescribing software gives clinics and hospitals the flexibility to design workflows around real prescribing patterns, not generic templates.
Workflow-Driven Design
Custom e-prescribing software adapts to physicians’ routines, reducing manual steps and improving medication management efficiency.
Stronger Safety Controls
Advanced drug interaction checks, allergy alerts, and controlled substance safeguards help reduce prescription errors and improve patient safety.
Compliance-Ready Architecture
Tailored systems support HIPAA compliance, DEA regulations, and EPCS requirements without forcing unnecessary features.
Seamless Integrations
Custom solutions integrate seamlessly with Electronic Health Records, telehealth platforms, and pharmacy networks such as Surescripts.
Scalable and Future-Proof
Unlike free e-prescribing software, custom platforms scale with patient volume and evolving digital healthcare workflows.
With the right development partner, such as AppsRhino, healthcare providers can build secure, cloud-based e-prescribing systems that fit their practice today and grow with them tomorrow.
Regulations and Compliance for E-Prescribing Software
Healthcare isn’t just about care; it’s also about control. When it comes to e-prescribing software, there are strict laws that shape how it works.
These rules exist for one reason: safety.

Laws Supporting E-Prescribing
The Drug Enforcement Administration (DEA) regulates how controlled substances are prescribed electronically.
To ensure secure prescribing, they introduced Electronic Prescriptions for Controlled Substances (EPCS).
This standard enforces identity checks, two-factor authentication, and digital signatures.
HIPAA (Health Insurance Portability and Accountability Act) also plays a big role. It requires that any electronic prescribing software keep patient data secure.
That means encrypted records, secure logins, and full access control.
Why Compliance Matters
Picture a busy clinic where doctors handle hundreds of prescriptions a day.
Without proper systems, a single breach could expose the personal data of thousands. That’s a lawsuit waiting to happen.
Compliance helps avoid all that. It reduces legal risks, boosts patient trust, and keeps operations running smoothly.
But meeting compliance isn’t just about checking boxes. It’s about building secure systems.
What Secure Systems Must Include
The best e-prescribing software offers audit trails, automatic backups, and role-based access. Every action is tracked.
Nothing slips through the cracks. These features aren’t extras—they’re essentials.
If e-prescribing software doesn’t meet legal standards, it puts patients and providers at risk.
Staying compliant isn’t a choice—it’s the foundation of digital healthcare.
Challenges of E-Prescribing Software
While e-prescribing software improves safety and efficiency, healthcare providers should be aware of several practical challenges when adopting electronic prescribing systems.
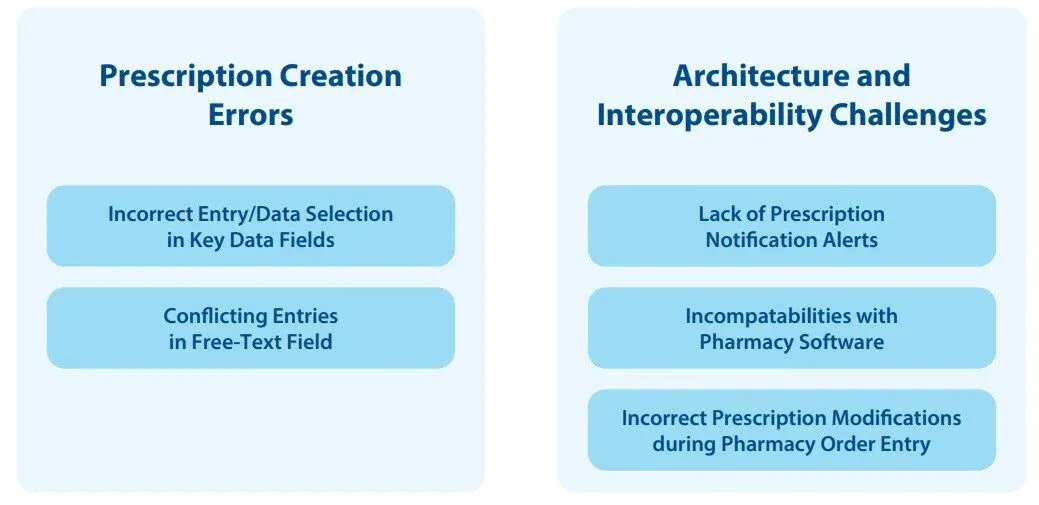
Learning Curve for Clinicians: Physicians transitioning from paper prescriptions may need time to adapt to electronic prescribing software, especially if the interface is complex or poorly designed.
Internet Dependency: Most eRx systems rely on a stable internet connection. Connectivity issues can delay electronic prescriptions, particularly in rural clinics or remote care settings.
System Errors or Downtime: As with any cloud-based healthcare software, technical glitches or outages can disrupt prescription delivery or require temporary workarounds.
Limited Pharmacy Compatibility: Not all pharmacies use the same electronic prescribing systems, which can affect seamless prescription routing and require manual intervention.
Integration Challenges: Integrating e-prescribing software with existing Electronic Health Records or billing systems can be complex without proper setup and support.
Controlled Substance Requirements: Prescribing controlled substances electronically requires additional steps under EPCS, which may increase setup time and compliance effort.
These challenges highlight the importance of choosing reliable, well-supported electronic prescribing software and providing proper training to ensure smooth, error-free digital healthcare workflows.
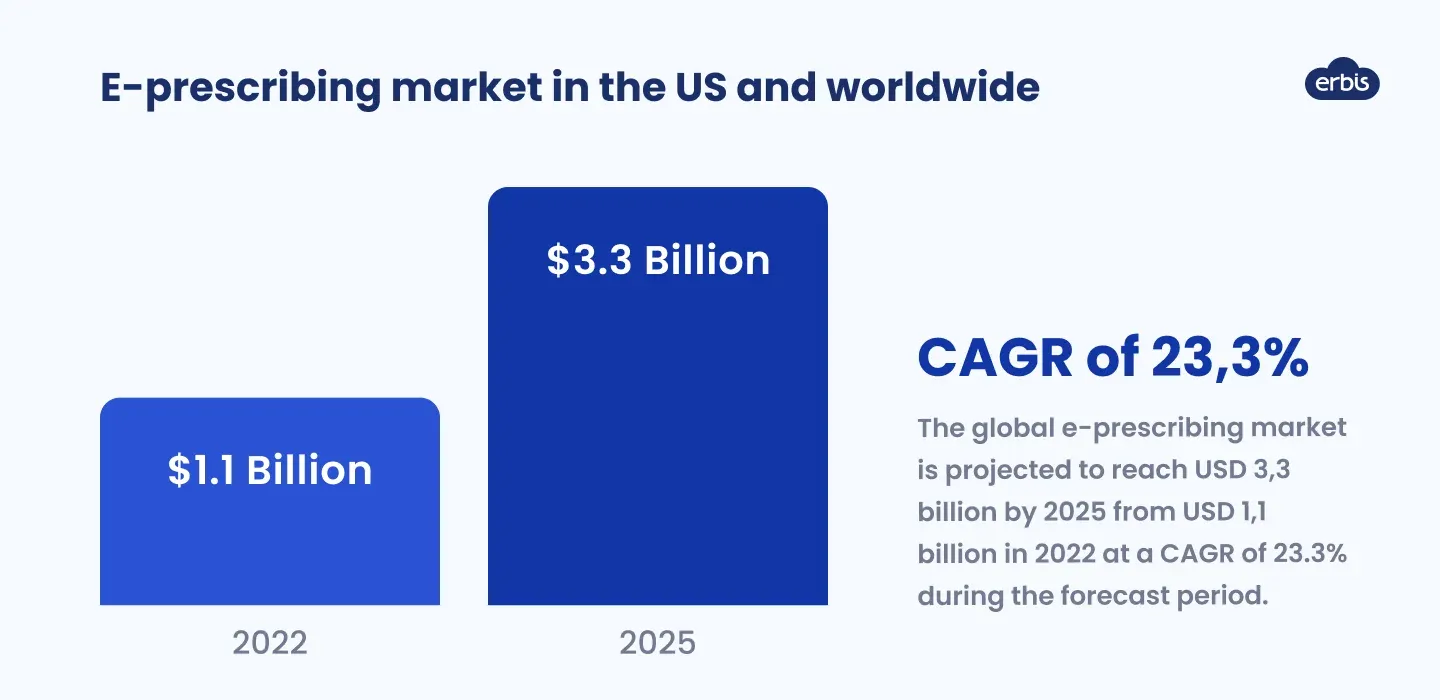
Future of E-Prescribing Software
The future of e-prescribing software looks smarter, faster, and more connected. And it’s already happening.
AI and Automation in Prescriptions
AI is starting to assist with decision-making. It can flag risky drug interactions and suggest safer alternatives.
Some systems even predict what a patient might need next—based on their medical history, allergies, and prescriptions.
This predictive prescribing reduces error and improves outcomes.
Integration with Telehealth and Mobile Apps
Mobile apps and telehealth are also changing the game. Patients can now consult doctors virtually and get prescriptions sent straight to their nearest pharmacy.
No travel. No paperwork. Just care on demand.
Predictive Prescribing Based on History
The ROI speaks for itself. Practices using modern electronic prescribing software report fewer errors and faster workflows.
This means happier patients and lower costs. In a world where convenience rules, digital prescribing is here to stay. And it’s only going to get better.
How to Choose the Right E-Prescribing Software
Choosing the right e-prescribing software directly affects patient safety, clinical efficiency, and long-term scalability.
Use this checklist to evaluate options clearly and confidently.
Selection Checklist for Healthcare Providers
- Ease of use: The electronic prescribing software should be intuitive, require minimal training, and fit naturally into daily clinical workflows.
- Safety features: Look for strong drug interaction checks, allergy alerts, and duplicate medication warnings to reduce prescription errors.
- Compliance readiness: Ensure the platform meets HIPAA compliance and supports DEA regulations, including Electronic Prescriptions for Controlled Substances (EPCS) if needed.
- System integration: The e-prescribing system should integrate smoothly with existing Electronic Health Records, billing tools, and pharmacy networks such as Surescripts.
- Reliability and uptime: Cloud-based healthcare software should include backup protocols and dependable support to avoid prescription delays.
- Scalability: Whether you start with free e-prescribing software or a paid plan, the system should scale with patient volume, providers, and telehealth prescribing needs.
Key Questions to Ask Vendors
- How long does staff onboarding and training typically take?
- Does the e-prescribing integration software work with our current EHR and pharmacy partners?
- What safeguards are in place during system outages or connectivity issues?
- What prescription data, refill patterns, or usage reports can we track?
- Are there additional costs for compliance features or future upgrades?
Evaluating electronic prescribing systems with this approach helps clinics and hospitals choose solutions that support safe care today and efficient digital healthcare workflows as they grow.
Conclusion
Paper prescriptions are going away, and that’s a good thing.
Today, e-prescribing software isn’t just a nice-to-have. It’s a must. It helps you move faster, stay compliant, and keep patients safe.
The right electronic prescribing software does more than replace pen-and-paper processes. It reduces errors, saves time, and streamlines your entire workflow.
In a world that’s only getting faster, digital prescriptions aren’t just the future. They’re the new normal.
And AppsRhino understands the need for tailored e-prescribing solutions.
Custom-built systems are designed to seamlessly fit your practice’s unique workflow, enhancing efficiency and reducing errors.
Focusing on creating solutions that not only meet industry standards but also align with the specific needs of your team and patients.
Frequently Asked Questions (FAQs)
Is e-prescribing software mandatory for physicians?
E-prescribing software is mandatory in many regions for controlled substances. Even when not required, electronic prescribing systems are widely adopted to improve compliance, safety, and efficiency.
Can e-prescribing software be used without an EHR?
Yes. Many e-prescribing software platforms operate independently or integrate lightly, making them suitable for clinics without a full Electronic Health Record.
How does e-prescribing software reduce prescription errors?
Electronic prescribing software uses standardized formats, drug interaction checks, and allergy alerts to prevent handwriting errors, incorrect dosages, and duplicate medications.
Is free e-prescribing software safe for clinical use?
Free e-prescribing software can be safe for basic prescribing, but advanced security, compliance, and scalability are often limited compared with paid or custom solutions.
What is required to prescribe controlled substances electronically?
Prescribing controlled substances requires EPCS compliance, including identity verification, secure authentication, and adherence to DEA regulations within the electronic prescribing system.
Table of Contents
- What is E-Prescribing Software?
- How E-Prescribing Software Works Step by Step
- Key Features of Modern E-Prescribing Software
- Benefits of E-Prescribing Software for Healthcare Providers
- Who Uses E-Prescribing Software and Why
- When Custom E-Prescribing Makes Sense
- Regulations and Compliance for E-Prescribing Software
- Challenges of E-Prescribing Software
- Future of E-Prescribing Software
- How to Choose the Right E-Prescribing Software
- Conclusion
- Frequently Asked Questions (FAQs)


